Common Sleep Disorders
Snoring
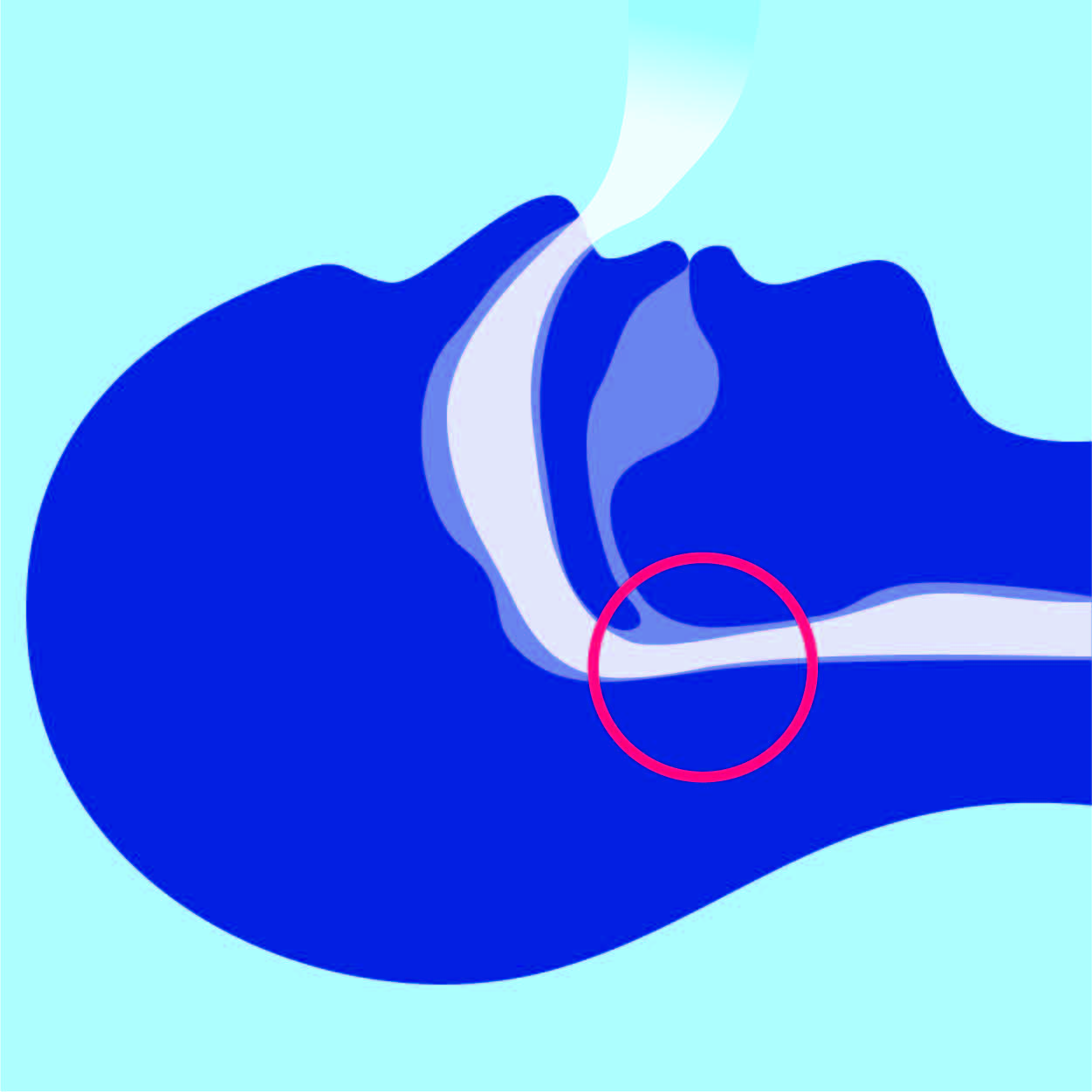
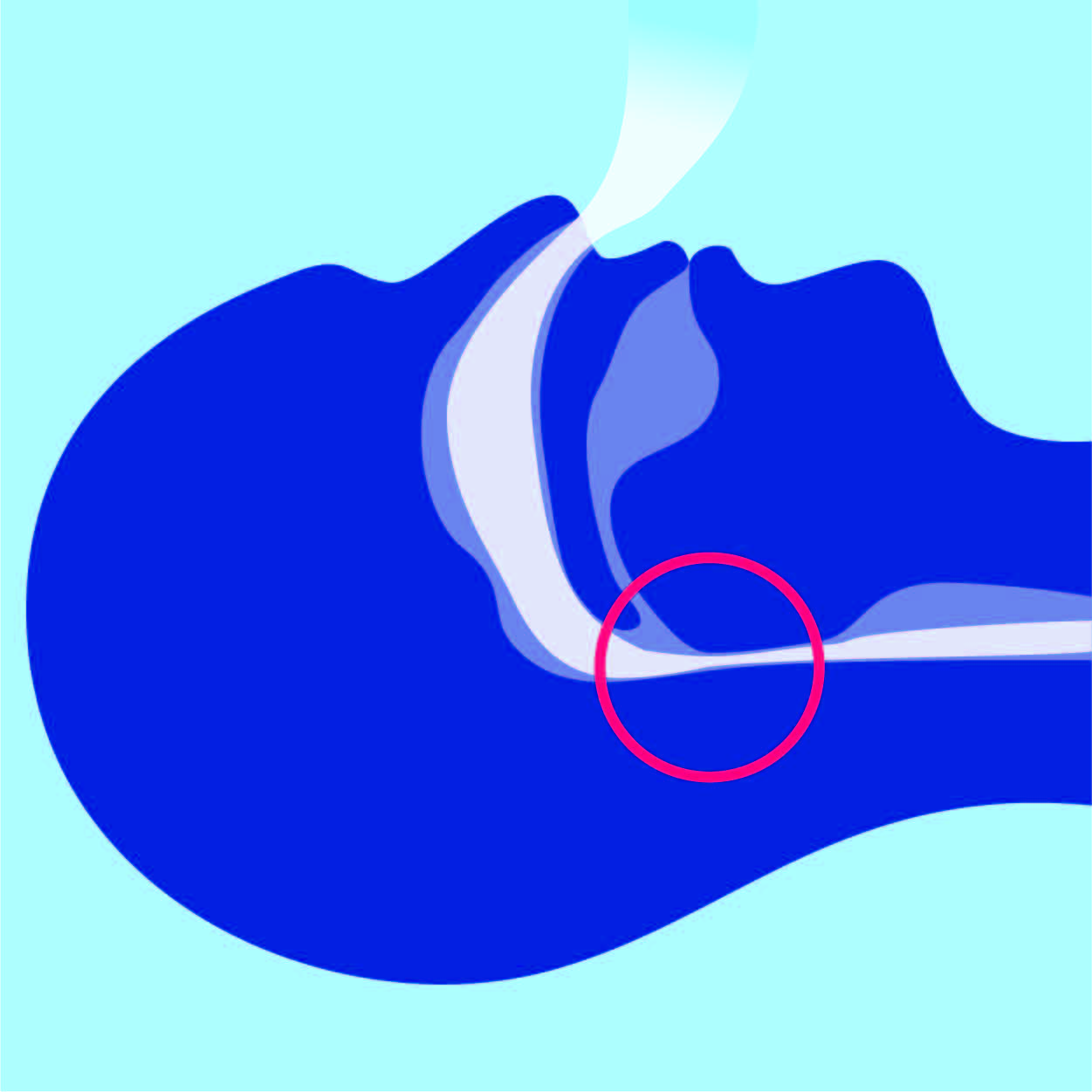
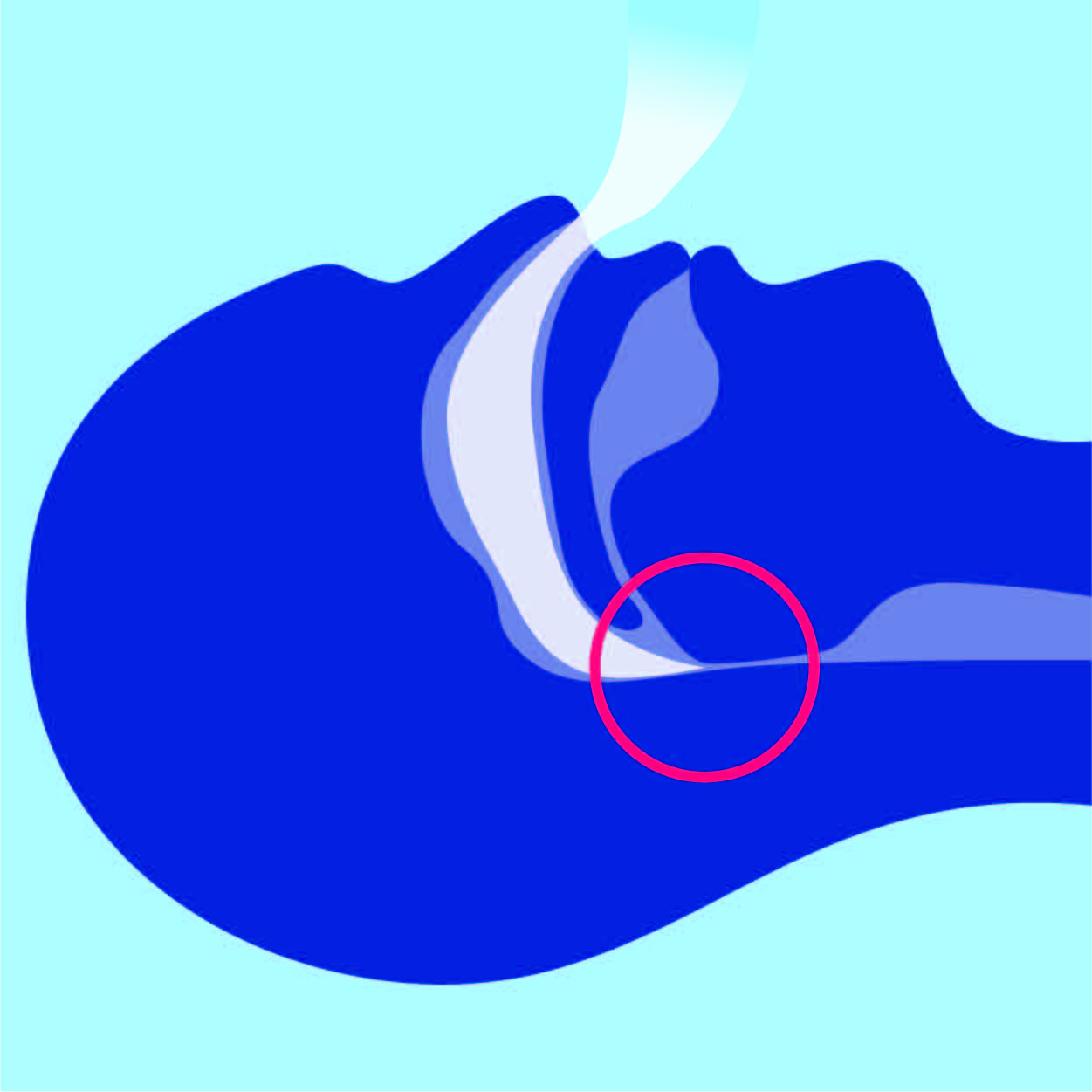
Snoring, and other noises at night such as gasping and choking are caused by your airways narrowing at the back of the throat as the brain is trying to rest at night. Snoring, gasping, popping noises, choking and stop/start breathing are all part of the snoring and sleep apnoea spectrum. They may just appear to be a nuisance to bed partners or roommates, but they are also indicative of a sleep disorder which will cause broken sleep with more awakenings then there should be, leading to lack of refreshment, tiredness and fatigue. Conservative treatments for snoring include overcoming potentially reversible factors, such as improving nasal congestion, perusing weight loss and modifying body positioning to more side and upright sleep.
There are also a number of over-the-counter type treatments which can be useful. More specialised treatments include mandibular advancement splints (custom made dental mouthguards), CPAP treatment, and selective surgeries targeting the nose or throat. An expert assessment usually includes sleep testing to ascertain the amount of abnormality and disruption to normal sleep. This then leads to a plan which can encompass basic manoeuvres addressing potentially reversible factors, as well as more specialised treatments appropriate for you.
Sleep Apnoea
Sleep apnoea is simply a name given to troubles with breathing at night as a result of snoring and narrowing of the throat. As we go to sleep, our brain relaxes control of the structures at the back of the throat and there is naturally a reduction in space. There are some factors that may predispose us to sleep apnoea such as getting older, carrying extra weight or having a blocked nose, amongst others. As a result, breathing may become laboured, which in turn causes subtle and at times major disruptions to the flow of breathing. Sleep is broken due to interruption to the brainwaves, which robs you of the refreshment that sleep should deliver.
Sleep apnoea is a step along but in the same spectrum as snoring. Most snorers have a degree of sleep apnoea but don’t know it. You can have sleep apnoea without obvious snoring as well. Furthermore, most people can’t recall what happens to them overnight and will often say swear there is nothing wrong, or if they do wake up at night or toss and turn, they will not remember the following morning.
There are a large proportion of thin people who have sleep apnoea, and they usually have a narrow throat structure. Thin and apparently healthy people who have sleep apnoea are often labeled as having chronic fatigue or depression when the real culprit is sleep apnoea and its variants. So the stereotype of being large or obese doesn’t apply to everyone.
A proper review of your complaints and bed partner observations, combined with a thorough examination and consideration of other contributory health issues is required. Testing in the form of an overnight sleep test is the best way to document the amount of abnormality and put a value on the disruption to brainwaves (sleep quality) and drops in oxygen. Although a minor degree of breathing abnormality at night can be considered normal, most people who think they have sleep apnoea will have more significant abnormalities which should be addressed.
Untreated sleep apnoea carries significant health implications such as changes in memory, mood, personality and vitality at one end of the spectrum, up to heart attacks, strokes, unstable diabetes, sudden death at night and even blindness at the other end.
Did you know that if you have untreated sleep apnoea and you are overweight, it is almost impossible to lose and sustain weight loss? Not only are you tired and failing to use up calories, your appetite centre has been programmed to increase food consumption, particularly the wrong types of foods (high calorie foods), increase your desire for snacks and increase your desire for food at the wrong times of day/night and in increasing amounts.
Untreated sleep apnoea has been shown to increase the chance of cardiovascular disease and death by up to 500%. This is because stress hormones are released, oxygen is lowered and blood pressure is raised. Blood is also more likely to congeal and blood vessels constrict to form clots. Arteries thicken and age prematurely with atherosclerosis. These physiological effects are magnified by the chronic degree of sleep deprivation.
Drivers with sleep apnoea are many times more likely to have a car accident and kill themselves or others as a result. This can be due to micro-sleeps which are hard to predict, as well as drowsiness and inattention. Accidents are more likely for those who drive for a living.
Untreated sleep apnoea leads to a lot of low-grade annoyance and suffering that is often hard to define. People will complain that their memory and thinking is not as clear, that there is a degree of grumpiness in the household and energy and application to work is diminished, particularly in the afternoons. Some people find it really hard to get up in the morning and shake off a sense of lack of refreshment and fatigue, despite what would be regarded as adequate time in bed the night before. Some wake up with a headache and a sense of fogginess like a hangover.
Effective treatments are available but the first step is to look at potentially reversible factors. Things such as weight loss, improving nasal patency, sleeping more upright and on your side, reviewing medications and any other obvious factors should be overcome at the outset. Treatment will be guided by a sleep test. More severe abnormalities should be treated promptly, while less severe abnormalities allow for time and basic manoeuvres to be undertaken. Further treatment options which can be organised are mandibular advancement splints, CPAP treatment and selective surgeries. A sleep disorder physician can tailor a plan that encompasses your wishes and the most fruitful treatment for your particular situation and state of health. There are a range of magic pills, potions and gadgets that are marketed within the community that are often clinically unproven and more commonly completely ineffective. It is important that a degree of caution is exercised before embarking on an expensive and unhelpful pathway.
NSD primarily tests for evidence of sleep apnoea. If you are experiencing any of the below symptoms, a consultation with a sleep specialist is advised.
Insomnia
Insomnia is a term used to describe when someone has difficulty initiating sleep or maintaining sleep. Most Australians will report insomnia at some point in their lives and at any one time, 30% of Australians are describing symptoms of insomnia. Insomnia is so common that it can be regarded as a natural part of life to some extent, but when it causes stress and trouble, it can be assessed, investigated and more often than not, treated effectively.
The emergence of the 24-hour society whereby we have less recreation time, are surrounded by distractions, light and noise, and the ability to entertain ourselves on our computers means that average sleep times are decreasing and good sleep habits are being forgotten. Insomnia treatment revolves around recognition of these factors and teasing out the causes that are relevant to you.
Insomnia has many faces. Some people are so overwhelmed by insomnia because it is so deeply ingrained. They may be completely addicted to tablets and certain habits which may in fact be counter-productive and haven’t provided them a cure. Other people will have worsening insomnia at certain times of stress. Typical groups affected by insomnia include women going through menopause, individuals going through bereavement or a life crisis and professionals who work indoors, particularly over the winter period.
It’s important to differentiate whether the insomnia is of a short duration or longer duration, what treatments have been trialed and what lifestyle and thought processes may be contributing to it. Looking at sleep patterns and identifying triggers and perpetuating influences on poor sleep is at the heart of insomnia assessment. From there, a treatment plan is formed to tackle the contributory and perpetuating factors, sometimes tackling them one by one. Often insomnia is linked in with other sleep disorders, such as snoring, poor sleep habits, sleep apnoea or restless legs. Sleep testing is usually performed at some stage to look at the interaction between these and to identify other factors which may contribute to insomnia. Other health issues that may impact on sleep can be addressed and improved such as hay fever, asthma, musculoskeletal and back discomfort, pain syndromes, depression, passing urine overnight, breathlessness, etc.
An appropriate treatment plan for insomnia is determined by the contributory and perpetuating factors mentioned above. It usually involves working with a sleep psychologist or sleep counsellor, overcoming medical factors, excluding other components such as sleep apnoea, in addition to improving habits and thought processes which are conducive to a better night’s sleep. The latest effective treatment is cognitive behavioural therapy (CBT), which has been shown to cure or improve people 80% of the time and get them off long term medications. Working with a sleep counsellor or sleep psychologist is therefore usually part of the treatment program. A review by a specialised sleep psychiatrist or neurologist to look for overwhelming anxiety or depressive symptoms is sometimes required.
Narcolepsy
Narcolepsy is an unusual condition with the typical stereotype being of a person sleeping throughout the day or falling asleep with little provocation, including falling asleep without warning (cataplexy). It has a genetic basis and can run in families. The cause of typical narcolepsy has been identified and specific treatments are currently being developed.
There are also a number of atypical forms of narcolepsy with people describing excessive sleepiness, tiredness and fatigue, despite adequate time in bed and no obvious cause for complaint. This is often termed idiopathic hypersomnolence and can overlap with chronic fatigue syndrome.
Narcolepsy is often underdiagnosed in our community. Specialist assessment and treatment is therefore the best way forward. A review of how it affects your daily life and whether it may be secondary to other sleep disorders has to be considered upfront, before treatments are prescribed.
Sleep testing is usually required to document the typical features of narcolepsy. This involves an overnight sleep study to look for other contributory conditions, with further monitoring the following morning in the form of a multiple sleep latency test (MSLT). Sometimes this needs to be repeated before a typical pattern of narcolepsy emerges.
As narcolepsy in its most severe forms can significantly impact the ability to maintain alertness, a full and frank discussion as to how it may affect your well-being and your livelihood is usually undertaken. Individuals in task critical occupations such as driving or materials handling may be at risk of harming themselves or others. The focus of narcolepsy treatment is to trial a stimulant medication of which there are two major types. Narcoleptics should take the necessary steps to keep themselves safe and work out a strategy for work and for driving. For the group of individuals who have a more severe form of narcolepsy where they fall asleep with little provocation, such as during the day or with emotional stimuli, further medication is usually trialed. Support groups are available but a reliance on postings on the Internet is often fraught with inaccuracy and inappropriate individual cases.
Restless legs & PLMS (Periodic Leg Movement Syndrome)
As the name suggests, restless legs are when someone has an annoying feeling in their legs or sometimes their arms and they feel compelled to move them to get some relief. When these occur at night they are termed periodic leg movement syndrome (PLMS) and can be readily identified with a diagnostic sleep study. Leg movements are often a marker that there is snoring and sleep apnoea but they may also coexist with insomnia. There are commonly used medications which can also bring on or worsen leg movements.
A proper assessment is initially undertaken to look at the effects of stress, psychological illness, relevant blood tests, as well as general and neurological health which may underlie leg movements. A sleep test is usually required to define the abnormality and determine whether it’s a primary or secondary issue. Thereafter, effective treatments depend somewhat on the underlying cause and involve basic manoeuvres, specific medications and/or rearrangement of medications. A nneurological assesment may be deemed necessary in some circumstances.
Poor sleep & other health conditions
Poor sleep can not only make you feel tired the following day, it can also significantly impact on your health. There are also other medical conditions which in turn can significantly impact on sleep so you have to work out which is which. Some of it is common sense, but this is where a sleep physician can come in and tease out what is the chicken and what is the egg.
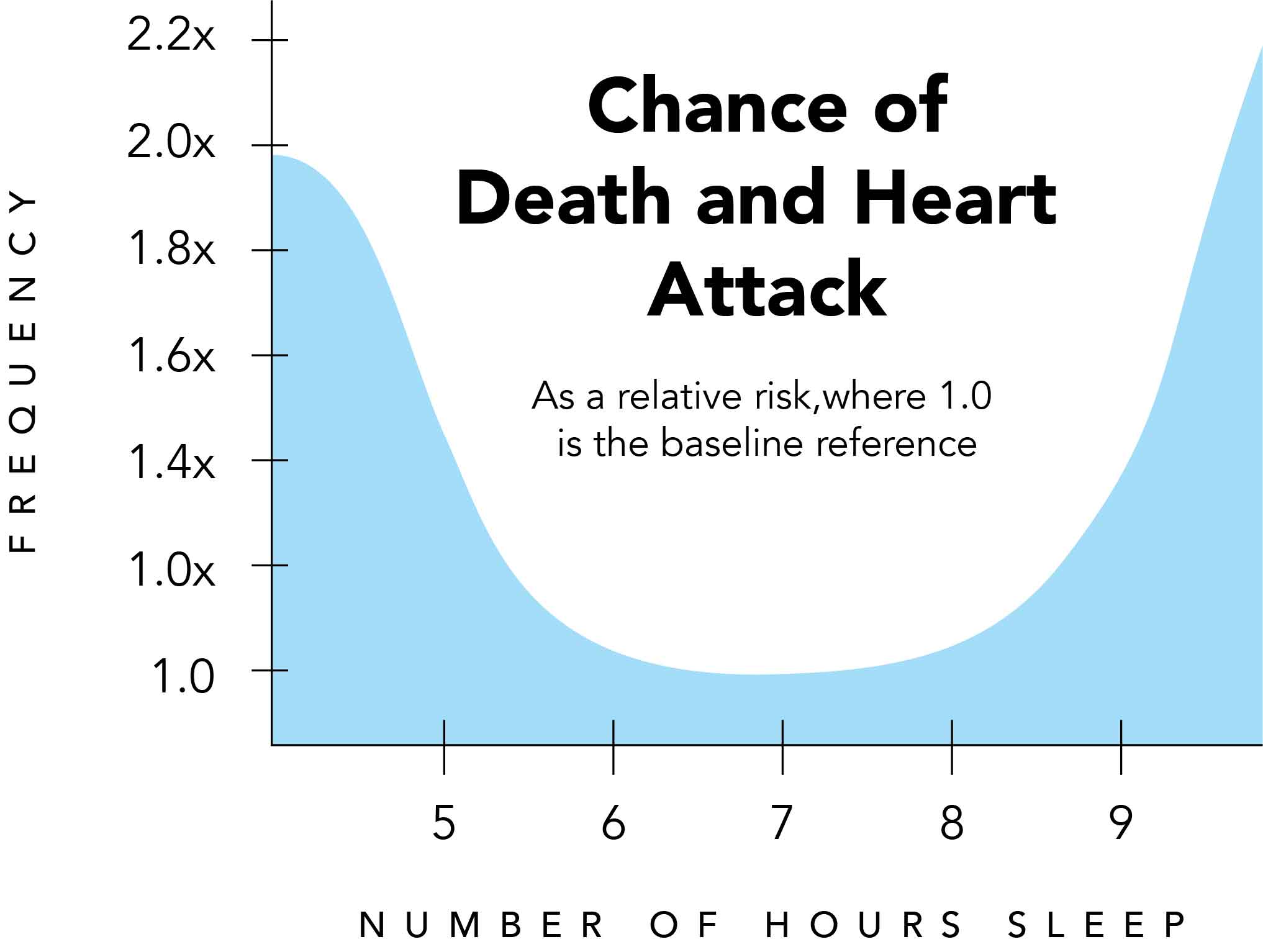
Did you know that there is a J shaped curve between the amount of sleep that you get and your chance of death? People who routinely get less than six hours sleep and those who routinely sleep for more than nine hours have a much higher chance of dying!
Getting less sleep than recommended, particulary less than six hours of sleep per night, dramatically increases your chance of death over time.
Sleep Apnoea and other conditions which increase sleepiness also raise rates of ill health and death... the more sleepy you are, the higher your chance of death.
Sleep deprivation causes agitation and activation of the stress hormone system and reduces the effectiveness of the immune system. For example, sleep deprivation leads to more frequent and repeated coughs and colds. The distress from sleep deprivation has been harnessed in torture techniques! Repeated or prolonged sleep deprivation such as that experienced during sleep apnoea will increase the chance of heart attack or stroke. Those who are sleep deprived are more prone to accidents, more likely to make erratic or poor choices and are often unpleasant to be around.
At the other end of the scale, the subtle effects of sleep disturbances such as sleep apnoea can slowly but surely alter our appetite so that we are more hungry, snack more and crave high energy foods, making weight loss that much more difficult. Significant sleep apnoea sufferers find it almost impossible to lose weight as a result.
However, there are many medical conditions which interact with sleep and can interfere or worsen it. Somewhat simple conditions such as arthritis with painful joints can make finding a comfortable bed position difficult. Our propensity towards eating later at night can lead to nocturnal reflux/heartburn. Other conditions that are often underestimated but can impact sleep if inadequately controlled overnight include hay fever, nasal obstruction and asthma. Parkinson’s disease can cause nightmares, insomnia and frequent movements, substantially interfering with sleep. This may make balancing medications more difficult.
The common use of various prescription medications can impact on sleep, such as frequently prescribed anti-agitation or depression medications, sleeping tablets or pain medications. Some common prescriptions can lead to nightmares, lack of energy and frequent leg movements.
Heart disease can often cause breathlessness at night. Irregular heartbeat and atrial fibrillation commonly occur overnight, and the period in the latter part of sleep leading to wakefulness is the most common time for a heart attack to start.
The combination of poor sleep and less than tiptop health such as being overweight, diabetic or hypertensive is now regarded as an epidemic, which contributes to further poor health, hospitalisation and health care utilisation, sudden death and accelerated chronic diseases, as well as absenteeism, road and transport accidents. These all lead to a major cost burden to our community.
Parasomnias & oddities
Unusual behaviours at night are given the name of parasomnias. In reality this is just a label or classification for some of the more common conditions which can affect sleep. These include common adult or childhood experiences such as nightmares, sleep talking, sleep walking, night terrors in children and bedwetting.
What’s more interesting and often a favourite in media reports, are odd or unusual behaviours termed non-REM parasomnia, or REM behaviour disorder. These can range from basic movements, vocalisations or actions, up to fairly complex behaviours such as going to the kitchen to make a sandwich, or acting out a dream. Often the movements can be quite violent such as kicking or punching. When the activity involves talking, it will look for all intents and purposes as deliberate. A particularly disturbing event is sleep paralysis, where individuals can be aware that they cannot move and this distressing situation can be fairly prolonged.
The root of these more interesting behaviours are generally due to a disconnection between the relaxed state of the brain and the muscles which control activity and actions. In addition, the emotional centre of the brain may burst out with activity which overwhelms the body’s relaxation at night. Depending on this mixture, people may or may not recall these events; they may be repetitive and frequent or just triggered occasionally by stressful events. Parasomnias frequently lead to broken and unrefreshing sleep, sometimes to self-harm and usually frightened bed partners or family members!
We are learning more about sleep as time goes on, and there seems to be a third portion of sleep where we are not fully awake or fully asleep and that is the time when parasomnias seem to be occurring. Recent media reports describing violent actions, sexual activity, driving and the effect of certain medications on sleep indicate that parasomnias are fairly common.
Parasomnias are frequently triggered by fairly common occurrences such as snoring and sleep apnoea, restless leg movements, psychological stress or agitating events, medications and some medical conditions such as Parkinson’s disease.
A full assessment would involve a detailed description of the events and their frequency, corroboration by bed partners or family members, review of contributory factors including medication usage, as well as sleep testing. In addition, a careful review of the role of mental stimulation, anxiety and agitation would be undertaken to help identify triggers for these behaviours.
Most parasomnias can be treated through basic interventions and ensuring that patients are kept safe. As the root cause of many of these is mental agitation, a sleep psychologist is often pivotal to help identify, control and remove triggers. Medications can be used to reduce severity. Some reduce the components of rapid eye movement sleep. Muscle relaxants reduce our body’s ability to respond or enact the dream, while sleep stabilising medications reduce the amount of disruption by reducing changes in sleep state. At a minimum, there would be a focus on adequate sleep and stress relief, including favourable sleep habits and light exposure.